How to Scale AI Without Breaking Your Infrastructure in 2025...
Read MoreThe Power of AI in Predicting Cardiovascular Disease: How papAI solution is Transforming Healthcare
Table of Contents
ToggleCardiovascular disease (CVD) is one of the most important causes of death in the world, so its prevention remains essential for humanity. According to the World Health Organisation (WHO), CVD causes an estimated 17.9 million deaths per year. This represents 32% of all deaths worldwide.
To diagnose CVD, a combination of laboratory tests, clinical symptoms, and risk factors is often used. However, the accuracy and reliability of these methods could be limited. The development of artificial intelligence (AI) technology has created new opportunities for improving CVD therapy and diagnostics.

By forecasting the risk of CVD, papAI solution is a great example of how AI-based technology is transforming healthcare. This ground-breaking approach applies AI algorithms to patient data analysis, including medical history, physical examination, and test findings, to provide individualized CVD risk ratings. The ability of AI to predict CVD will be discussed in this introduction along with how the papAI solution is changing healthcare by enhancing early detection, prevention, and treatment of CVD.
What are cardiovascular diseases?
The categories of diseases known as cardiovascular disease (CVD) are diseases that damage the heart and blood arteries. When a build-up of plaque causes the arteries that carry blood to the heart and brain to narrow or become blocked, CVD can result. A heart attack or stroke can then occur. The medical specialists have identified 6 types:
1- One common type of CVD is coronary heart disease, which is a disease of the blood vessels supplying the heart muscle. This condition can lead to chest pain, heart attacks, and other serious complications.
2- Another type of CVD is cerebrovascular disease, which is a disease of the blood vessels supplying the brain. This can lead to strokes, which can cause brain damage and other long-term complications.
3- Peripheral arterial disease is another type of CVD that affects the blood vessels supplying the arms and legs. This condition can cause pain, numbness, and other symptoms, and can lead to serious complications if left untreated.
4- Rheumatic heart disease is a type of CVD that is caused by damage to the heart muscle and heart valves from rheumatic fever, which is caused by streptococcal bacteria. This condition can lead to heart failure, arrhythmias, and other serious complications.
5- Congenital heart disease is a type of CVD that affects individuals from birth. It is caused by malformations of the heart structure during development and can lead to a range of complications, depending on the specific defect.
6- Finally, deep vein thrombosis and pulmonary embolism are conditions that occur when blood clots form in the leg veins and dislodge, moving to the heart and lungs. These conditions can be life-threatening if left untreated.
What are the risk factors for cardiovascular disease?
Cardiovascular disease (CVD) risk factors come in a variety of forms, some of which are controllable and others of which are not. Individuals can minimize their chance of having CVD by taking action after becoming aware of these risk factors. The following are the main CVD risk factors:
1- Age
The risk of developing CVD increases with age. This is because with age, blood vessels can become stiffer and less flexible, making it more difficult for blood to flow. In addition, the build-up of plaque in the arteries over time can lead to atherosclerosis, a key factor in CVD. Although CVD can happen at any age. The American Heart Association estimates that 34% of CVD fatalities in adults 75 and older occur in this age group. In addition, at the age of 55, the chance of having a heart attack and having a stroke doubles.
2- Family history
Family history (CVD) is another unchangeable risk factor for cardiovascular disease. The risk of developing CVD can increase if there is a family history, especially if a close relative (parent or sibling) suffered from the disease while still quite young (before the age of 55 for men, and before the age of 65 for women). It is thought that both genetic and environmental factors contribute to the elevated risk of CVD linked with a family history. According to current thinking, certain genetic variations can be passed down from one generation to the next and may make a person more likely to develop CVD.
3- Smoking
One of the major modifiable risk factors for cardiovascular disease is smoking (CVD). Inflammation, damage to the lining of blood vessels and the build-up of plaque in the arteries are all effects of the chemicals in cigarette smoke. Heart attacks, strokes and other CVD-related problems may increase as a result. One of the most crucial things people can do to lower their chances of having CVD is to stop smoking. After a year of stopping smoking, the risk of getting cardiovascular disease (CVD) considerably lowers, according to the American Heart Association. The risk of stroke can be decreased to that of a non-smoker in 2–5 years, and the risk of heart attack can be decreased to that of a non-smoker in 5–15 years.
4- Diabetes
A significant modifiable risk factor for cardiovascular disease is diabetes (CVD). Diabetes raises a person’s risk of coronary heart disease, stroke, and peripheral artery disease, among other CVD. Although the precise processes by which diabetes raises the risk of CVD are still unclear, it is believed that these mechanisms are linked to the effects of elevated blood sugar on the blood arteries. High blood sugar levels over time can harm blood vessel linings, making them less flexible and more prone to plaque accumulation. High blood pressure and high cholesterol are two additional CVD risk factors that can be exacerbated by high blood sugar.
5- Obesity
Excess body weight can lead to other risk factors for CVD, including high blood pressure, high cholesterol, and diabetes. It can also contribute to the buildup of plaque in the arteries, which can increase the risk of heart attack and stroke. For example, excess body fat can lead to insulin resistance and the release of inflammatory chemicals, both of which can contribute to the development of CVD.
How AI-based solutions can help detect CVD
Machine learning, deep learning, and natural language processing are just a few of the technologies that go under the umbrella term of artificial intelligence (AI). With the use of these technologies, computers are now able to learn from large data and base predictions or choices on that learning. AI may be used to examine a variety of data sources, including genetic information, electronic health records, and medical imaging in the context of CVD in order to spot trends and forecast a patient’s likelihood of acquiring the disease.
The use of machine learning algorithms to assess medical imaging data, such as computed tomography (CT) scans and magnetic resonance imaging (MRI) scans, is one application of AI in CVD diagnosis. Even before symptoms appear, these algorithms can identify small alterations in the heart and blood vessels that may be early signals of CVD. This may allow for early diagnosis and treatment, improving patient outcomes.
Electronic health information may be analyzed using AI to find people who are at high risk for cardiovascular disease. AI algorithms are able to find patterns linked to a higher risk of CVD by examining a significant quantity of data, including patient demographics, medical history, and test findings. This can help medical professionals focus their interventions on the people who will benefit from them the most, increasing the efficacy and efficiency of efforts to prevent CVD.
Using genetic data to recognize people with a high risk of developing CVD is another way AI is used to diagnose CVD. AI systems can identify people who are more likely to develop CVD by examining genetic markers linked to the condition. This can make it possible for tailored treatments, such as dietary adjustments or drug therapy, to lower the risk of CVD in high-risk individuals.
How AI impacts clinical decision making
healthcare is a strategic field for artificial intelligence. It is characterized by the complexity of the data to be analyzed, the large number of variables to be taken into account and the importance of accurate diagnoses to reduce medical errors and improve the quality of care.
What does papAI solution provide?
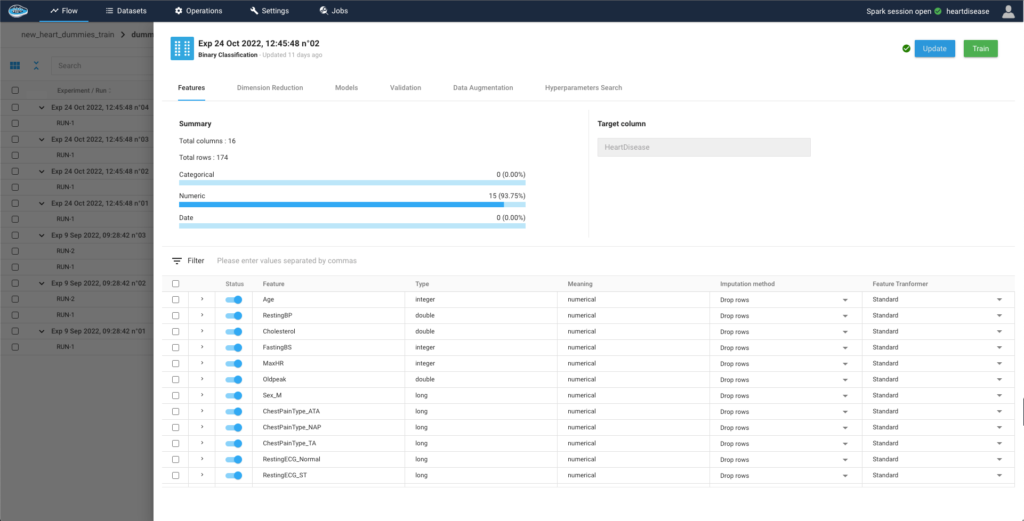
In this study, we used data from patients with characteristics such as vital signs and medical history to predict whether they will potentially develop cardiovascular disease.
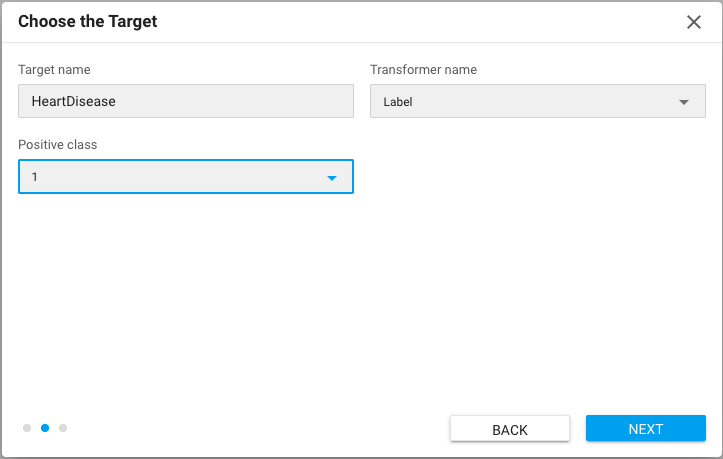
1- Identifying the target
The objective in our situation is to forecast the occurrence of any cardiac disease in a certain group. A person must be classified as having a disease risk if a favorable outcome occurs. The risk factors for developing it can then be determined.
2- Configure the models
The selection of features is the first step in building our model, allowing us to understand how they relate to the target and incorporate that knowledge into the model training.
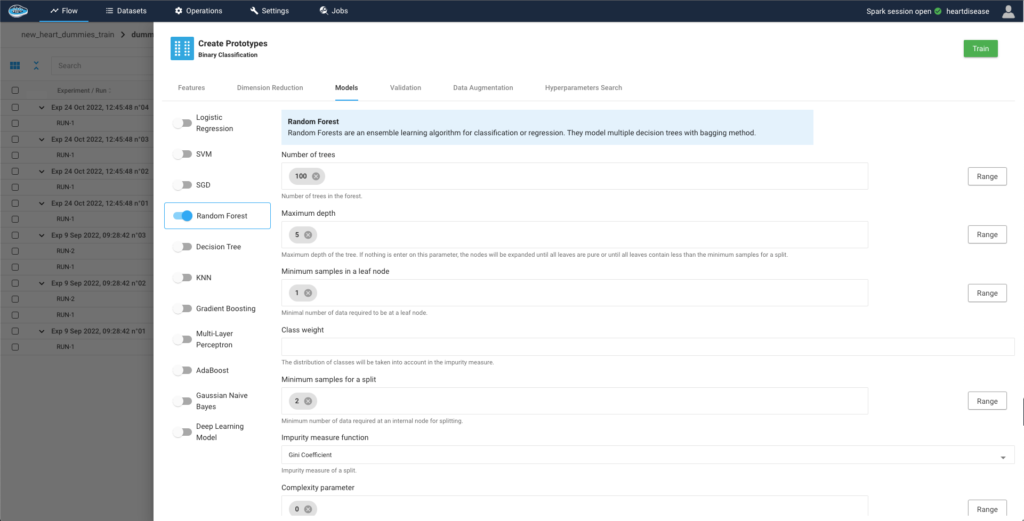
Afterwards, we select the models that could be compatible with the problem we want to solve. papAI integrates a large catalogue of ready-to-use models to easily build, train and deploy an AI pipeline. For more complex projects, papAI also provides an AutoML feature
3- Evaluate the trained experiments
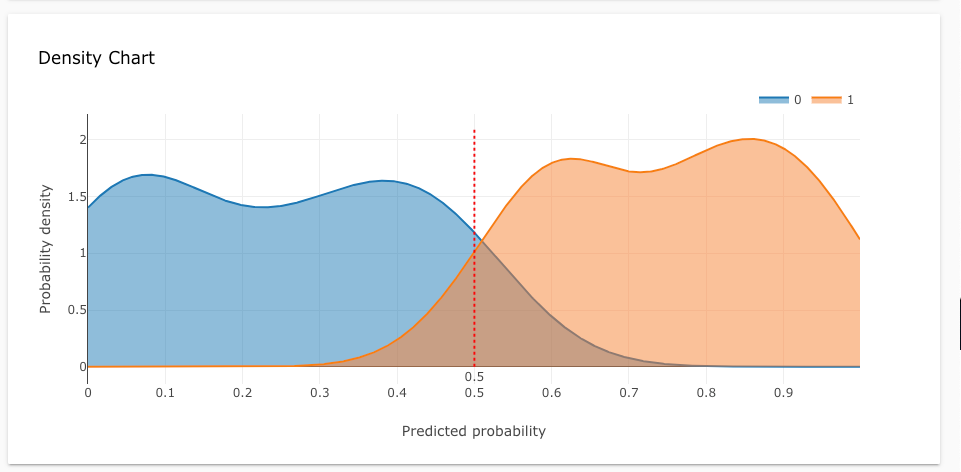
After running an experiment comes the evaluation process. We must identify its effectiveness and its performance when predicting the target through a series of metrics implemented into papAI’s interface. For example, evaluation metrics include accuracy, density chart, confusion matrix …
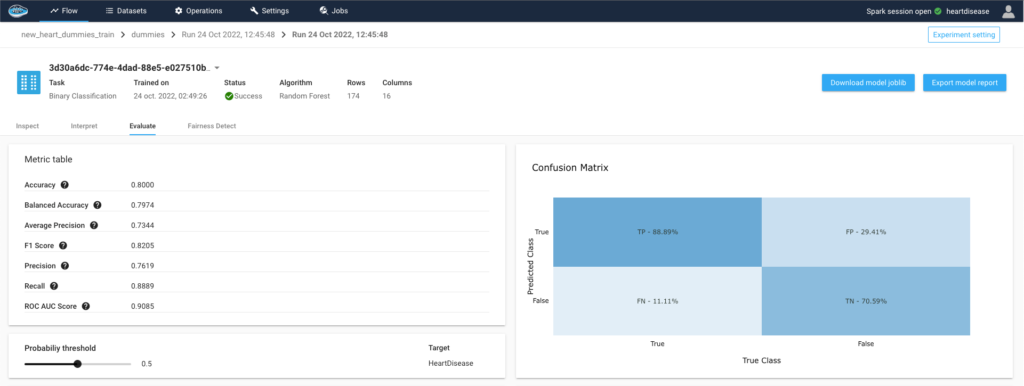
Through the density chart we can clearly see the ability for the model to determine the difference between both classes, people with or without heart disease, at a median threshold of 0.5, meaning that model successfully detected the two population independently.
4- Interpret the predicted outcome
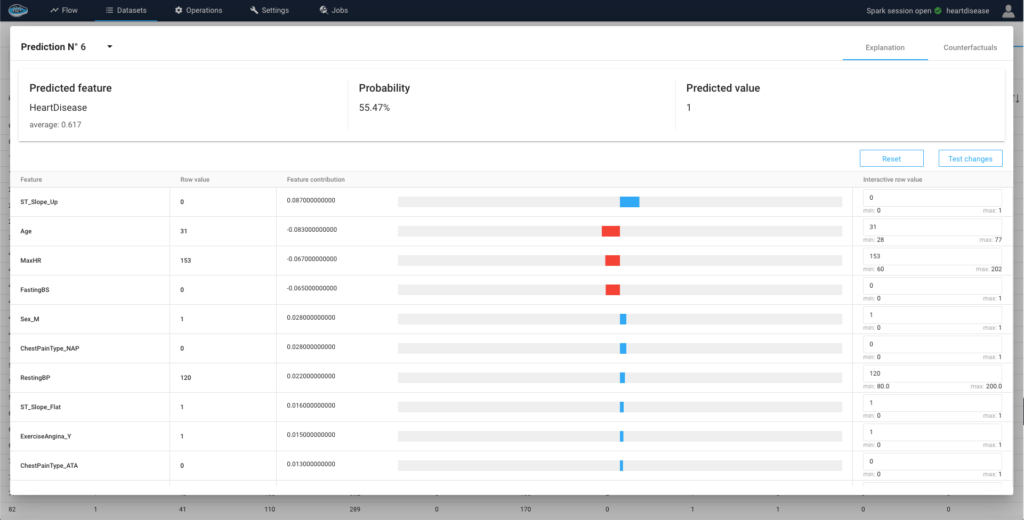
The evaluation process goes along with the explainability part to understand the model’s behaviour and the influence of each variable on the prediction’s probability. We can then assess the probable risk factors of having an heart disease.

After going through these important processes, a model is chosen and promoted in order to apply it on an testing dataset and obtain individual predictions with a local interpretability. Thanks to this local interpretability, we can deeply understand the decision made by the model and try to develop cases to modify the predicted outcome.
Conlcusion
Patient treatment by doctors may be delayed due to organizational and structural problems, which would increase mortality. It is therefore essential to identify people at risk earlier so that they can receive faster and more specialized care. papAI solution offers practical help in identifying patients with cardiovascular disease through a method that provides a high level of explicability of results by identifying the factors that need to be monitored most effectively.
If you’re interested in learning more about the papAI platform and how it can help you build your own tool, you can book a demo with one of our AI experts. Our team can show you how the platform works and help you get started on your own.
Interested in discovering papAI?
Our commercial team is at your disposal for any questions.
“DATATEGY EARLY CAREERS PROGRAM” With Noé Vartanian
“DATATEGY EARLY CAREERS PROGRAM” With Noé Vartanian Hello all, my...
Read MoreUse AI to Predict Your Customer’s Future Value
Use AI to Predict Your Customer’s Future Value Understanding and...
Read MoreHow Geospatial Analytics Transforms Decision-Making
How Geospatial Analytics Transforms Decision-Making Making the right judgments in...
Read More


